Search
- Page Path
- HOME > Search
- Thyroid
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
- Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
- Endocrinol Metab. 2024;39(1):47-60. Published online February 15, 2024
- DOI: https://doi.org/10.3803/EnM.2024.1937
- 1,905 View
- 173 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
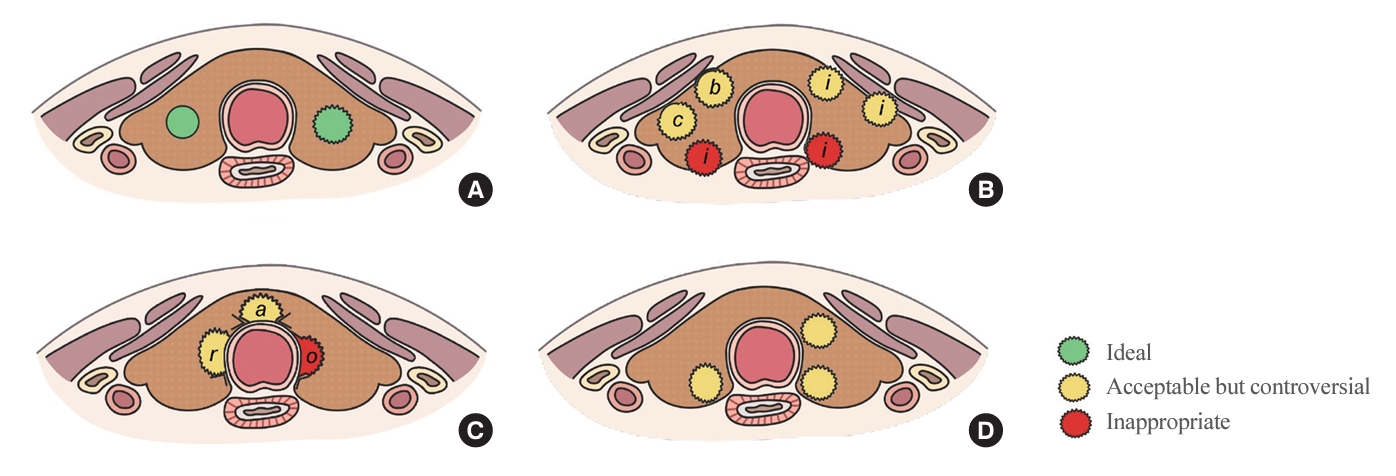
ePub - The indolent nature and favorable outcomes associated with papillary thyroid microcarcinoma have prompted numerous prospective studies on active surveillance (AS) and its adoption as an alternative to immediate surgery in managing low-risk thyroid cancer. This article reviews the current status of AS, as outlined in various international practice guidelines. AS is typically recommended for tumors that measure 1 cm or less in diameter and do not exhibit aggressive subtypes on cytology, extrathyroidal extension, lymph node metastasis, or distant metastasis. To determine the most appropriate candidates for AS, factors such as tumor size, location, multiplicity, and ultrasound findings are considered, along with patient characteristics like medical condition, age, and family history. Moreover, shared decision-making, which includes patient-reported outcomes such as quality of life and cost-effectiveness, is essential. During AS, patients undergo regular ultrasound examinations to monitor for signs of disease progression, including tumor growth, extrathyroidal extension, or lymph node metastasis. In conclusion, while AS is a feasible and reliable approach for managing lowrisk thyroid cancer, it requires careful patient selection, effective communication for shared decision-making, standardized follow-up protocols, and a clear definition of disease progression.

- Diabetes, obesity and metabolism
- Triglyceride-Glucose Index Predicts Future Atherosclerotic Cardiovascular Diseases: A 16-Year Follow-up in a Prospective, Community-Dwelling Cohort Study
- Joon Ho Moon, Yongkang Kim, Tae Jung Oh, Jae Hoon Moon, Soo Heon Kwak, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi, Nam H. Cho
- Endocrinol Metab. 2023;38(4):406-417. Published online August 3, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1703
- 2,678 View
- 166 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
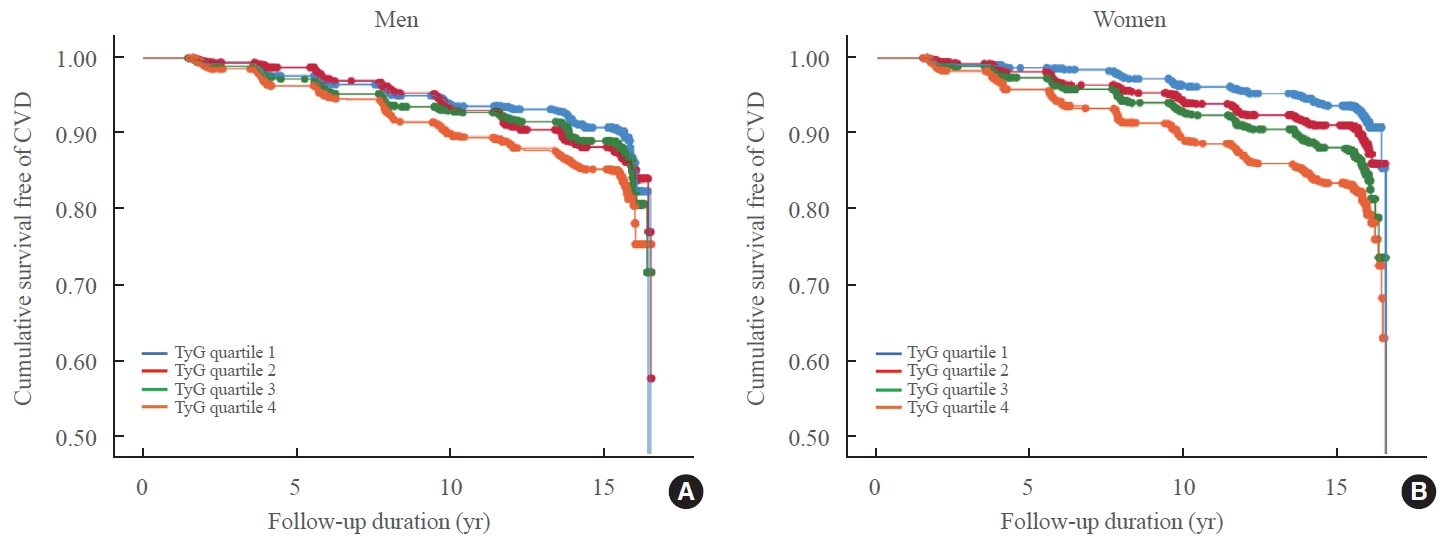
ePub - Background
While the triglyceride-glucose (TyG) index is a measure of insulin resistance, its association with cardiovascular disease (CVD) has not been well elucidated. We evaluated the TyG index for prediction of CVDs in a prospective large communitybased cohort.
Methods
Individuals 40 to 70 years old were prospectively followed for a median 15.6 years. The TyG index was calculated as the Ln [fasting triglycerides (mg/dL)×fasting glucose (mg/dL)/2]. CVDs included any acute myocardial infarction, coronary artery disease or cerebrovascular disease. We used a Cox proportional hazards model to estimate CVD risks according to quartiles of the TyG index and plotted the receiver operating characteristics curve for the incident CVD.
Results
Among 8,511 subjects (age 51.9±8.8 years; 47.5% males), 931 (10.9%) had incident CVDs during the follow-up. After adjustment for age, sex, body mass index, diabetes mellitus, hypertension, total cholesterol, smoking, alcohol, exercise, and C-reactive protein, subjects in the highest TyG quartile had 36% increased risk of incident CVD compared with the lowest TyG quartile (hazard ratio, 1.36; 95% confidence interval, 1.10 to 1.68). Carotid plaque, assessed by ultrasonography was more frequent in subjects in the higher quartile of TyG index (P for trend=0.049 in men and P for trend <0.001 in women). The TyG index had a higher predictive power for CVDs than the homeostasis model assessment of insulin resistance (HOMA-IR) (area under the curve, 0.578 for TyG and 0.543 for HOMA-IR). Adding TyG index on diabetes or hypertension alone gave sounder predictability for CVDs.
Conclusion
The TyG index is independently associated with future CVDs in 16 years of follow-up in large, prospective Korean cohort. -
Citations
Citations to this article as recorded by- Construction and validation of a nomogram for predicting diabetes remission at 3 months after bariatric surgery in patients with obesity combined with type 2 diabetes mellitus
Kaisheng Yuan, Bing Wu, Ruiqi Zeng, Fuqing Zhou, Ruixiang Hu, Cunchuan Wang
Diabetes, Obesity and Metabolism.2024; 26(1): 169. CrossRef - Association between the triglyceride glucose index and chronic total coronary occlusion: A cross-sectional study from southwest China
Kaiyong Xiao, Huili Cao, Bin Yang, Zhe Xv, Lian Xiao, Jianping Wang, Shuiqing Ni, Hui Feng, Zhongwei He, Lei Xv, Juan Li, Dongmei Xv
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(4): 850. CrossRef - The association between TyG and all-cause/non-cardiovascular mortality in general patients with type 2 diabetes mellitus is modified by age: results from the cohort study of NHANES 1999–2018
Younan Yao, Bo Wang, Tian Geng, Jiyan Chen, Wan Chen, Liwen Li
Cardiovascular Diabetology.2024;[Epub] CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Evaluation of the novel three lipid indices for predicting five- and ten-year incidence of cardiovascular disease: findings from Kerman coronary artery disease risk factors study (KERCADRS)
Alireza Jafari, Hamid Najafipour, Mitra Shadkam, Sina Aminizadeh
Lipids in Health and Disease.2023;[Epub] CrossRef
- Construction and validation of a nomogram for predicting diabetes remission at 3 months after bariatric surgery in patients with obesity combined with type 2 diabetes mellitus

- Miscellaneous
- Corrigendum: Correction of Acknowledgments. Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2022;37(1):181-182. Published online February 28, 2022
- DOI: https://doi.org/10.3803/EnM.2022.104
- Corrects: Endocrinol Metab 2021;36(2):359
- 2,804 View
- 110 Download
- 1 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study
Sungho Bea, Heejun Son, Jae Hyun Bae, Sun Wook Cho, Ju‐Young Shin, Young Min Cho
Diabetes, Obesity and Metabolism.2024; 26(1): 108. CrossRef
- Risk of thyroid cancer associated with glucagon‐like peptide‐1 receptor agonists and dipeptidyl peptidase‐4 inhibitors in patients with type 2 diabetes: A population‐based cohort study

- Thyroid
- Association between Thyroid Function and Heart Rate Monitored by Wearable Devices in Patients with Hypothyroidism
- Ki-Hun Kim, Juhui Lee, Chang Ho Ahn, Hyeong Won Yu, June Young Choi, Ho-Young Lee, Won Woo Lee, Jae Hoon Moon
- Endocrinol Metab. 2021;36(5):1121-1130. Published online October 21, 2021
- DOI: https://doi.org/10.3803/EnM.2021.1216

- 5,430 View
- 157 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Heart rate (HR) monitored by a wearable device (WD) has demonstrated its clinical feasibility for thyrotoxicosis subjects. However, the association of HR monitored by wearables with hypothyroidism has not been examined. We assessed the association between serum thyroid hormone concentration and three WD-HR parameters in hypothyroid subjects.
Methods
Forty-four subjects scheduled for radioactive iodine therapy (RAI Tx) after thyroid cancer surgery were included. Thirty subjects were prepared for RAI Tx by thyroid hormone withdrawal (hypothyroidism group) and 14 subjects by recombinant human thyrotropin (control group). Three WD-HR parameters were calculated from the HR data collected during rest, during sleep, and from 2:00 AM to 6:00 AM, respectively. We analyzed the changes in conventionally measured resting HR (On-site rHR) and WDHR parameters relative to thyroid hormone levels.
Results
Serum free thyroxine (T4) levels, On-site rHR, and WD-HR parameters were lower in the hypothyroid group than in the control group at the time of RAI Tx. WD-HR parameters also reflected minute changes in free T4 levels. A decrease in On-site rHR and WD-HR parameters by one standard deviation (On-site rHR, approximately 12 bpm; WD-HR parameters, approximately 8 bpm) was associated with a 0.2 ng/dL decrease in free T4 levels (P<0.01) and a 2-fold increase of the odds ratio of hypothyroidism (P<0.01). WD-HR parameters displayed a better goodness-of-fit measure (lower quasi-information criterion value) than On-site rHR in predicting the hypothyroidism.
Conclusion
This study identified WD-HR parameters as informative and easy-to-measure biomarkers to predict hypothyroidism. -
Citations
Citations to this article as recorded by- Application of wearables for remote monitoring of oncology patients: A scoping review
Katharina Cloß, Marlo Verket, Dirk Müller-Wieland, Nikolaus Marx, Katharina Schuett, Edgar Jost, Martina Crysandt, Fabian Beier, Tim H Brümmendorf, Guido Kobbe, Julia Brandts, Malte Jacobsen
DIGITAL HEALTH.2024;[Epub] CrossRef - Thyroid hormone action during GABAergic neuron maturation: The quest for mechanisms
Sabine Richard, Juan Ren, Frédéric Flamant
Frontiers in Endocrinology.2023;[Epub] CrossRef - A machine learning-assisted system to predict thyrotoxicosis using patients’ heart rate monitoring data: a retrospective cohort study
Kyubo Shin, Jongchan Kim, Jaemin Park, Tae Jung Oh, Sung Hye Kong, Chang Ho Ahn, Joon Ho Moon, Min Joo Kim, Jae Hoon Moon
Scientific Reports.2023;[Epub] CrossRef
- Application of wearables for remote monitoring of oncology patients: A scoping review

- Clinical Study
- Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
- Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
- Endocrinol Metab. 2021;36(2):359-364. Published online March 23, 2021
- DOI: https://doi.org/10.3803/EnM.2020.890
- Correction in: Endocrinol Metab 2022;37(1):181

- 5,800 View
- 202 Download
- 17 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
A Korean Multicenter Prospective cohort study of Active Surveillance or Surgery (KoMPASS) for papillary thyroid microcarcinomas (PTMCs) has been initiated. The aim is to compare clinical outcomes between active surveillance (AS) and an immediate lobectomy for low-risk PTMCs. We here outline the detailed protocol for this study.
Methods
Adult patients with a cytopathologically confirmed PTMC sized 6.0 to 10.0 mm by ultrasound (US) will be included. Patients will be excluded if they have a suspicious extra-thyroidal extension or metastasis of a PTMC or multiple thyroid nodules or other thyroid diseases which require a total thyroidectomy. Printed material describing the prognosis of PTMCs, and the pros and cons of each management option, will be provided to eligible patients to select their preferred intervention. For the AS group, thyroid US, thyroid function, and quality of life (QoL) parameters will be monitored every 6 months during the first year, and then annually thereafter. Disease progression will be defined as a ≥3 mm increase in maximal diameter of a PTMC, or the development of new thyroid cancers or metastases. If progression is detected, patients should undergo appropriate surgery. For the lobectomy group, a lobectomy with prophylactic central neck dissection will be done within 6 months. After initial surgery, thyroid US, thyroid function, serum thyroglobulin (Tg), anti-Tg antibody, and QoL parameters will be monitored every 6 months during the first year and annually thereafter. Disease progression will be defined in these cases as the development of new thyroid cancers or metastases.
Conclusion
KoMPASS findings will help to confirm the role of AS, and develop individualized management strategies, for low-risk PTMCs. -
Citations
Citations to this article as recorded by- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines
Min Joo Kim, Jae Hoon Moon, Eun Kyung Lee, Young Shin Song, Kyong Yeun Jung, Ji Ye Lee, Ji-hoon Kim, Kyungsik Kim, Sue K. Park, Young Joo Park
Endocrinology and Metabolism.2024; 39(1): 47. CrossRef - It Is Time to Understand the Additional Benefits of Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Kyeong Jin Kim
Endocrinology and Metabolism.2024; 39(1): 95. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Active Surveillance for Low-Risk Papillary Thyroid Carcinoma as an Acceptable Management Option with Additional Benefits: A Comprehensive Systematic Review
Jee Hee Yoon, Wonsuk Choi, Ji Yong Park, A Ram Hong, Hee Kyung Kim, Ho-Cheol Kang
Endocrinology and Metabolism.2024; 39(1): 152. CrossRef - Thyroid‐Stimulating Hormone, Age, and Tumor Size are Risk Factors for Progression During Active Surveillance of Low‐Risk Papillary Thyroid Microcarcinoma in Adults
Yasuhiro Ito, Akira Miyauchi, Makoto Fujishima, Takuya Noda, Tsutomu Sano, Takahiro Sasaki, Taketoshi Kishi, Tomohiko Nakamura
World Journal of Surgery.2023; 47(2): 392. CrossRef - Thyroid FNA cytology: The Eastern versus Western perspectives
Mitsuyoshi Hirokawa, Manon Auger, Chan Kwon Jung, Fabiano Mesquita Callegari
Cancer Cytopathology.2023; 131(7): 415. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - Long-Term Outcomes of Active Surveillance and Immediate Surgery for Adult Patients with Low-Risk Papillary Thyroid Microcarcinoma: 30-Year Experience
Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Akihiro Miya, Naoyoshi Onoda, Minoru Kihara, Takuya Higashiyama, Hiroo Masuoka, Shiori Kawano, Takahiro Sasaki, Mitsushige Nishikawa, Shuji Fukata, Takashi Akamizu, Mitsuru Ito, Eijun Nishihara, Mako Hisakad
Thyroid®.2023; 33(7): 817. CrossRef - Active Surveillance Outcomes of Patients with Low-Risk Papillary Thyroid Microcarcinoma According to Levothyroxine Treatment Status
Masashi Yamamoto, Akira Miyauchi, Yasuhiro Ito, Makoto Fujishima, Takahiro Sasaki, Takumi Kudo
Thyroid®.2023; 33(10): 1182. CrossRef - Cost-Effectiveness of Active Surveillance Compared to Early Surgery of Small Papillary Thyroid Cancer: A Retrospective Study on a Korean Population
Han-Sang Baek, Jeonghoon Ha, Kwangsoon Kim, Jaseong Bae, Jeong Soo Kim, Sungju Kim, Dong-Jun Lim, Chulmin Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Optimal Cutoff Values of the Contact Angle of Tumor on Sonography System for Predicting Extrathyroidal Extension of Papillary Thyroid Carcinoma by Tumor Location
Ik Beom Shin, Do Hoon Koo, Dong Sik Bae
Clinical Medicine Insights: Oncology.2023;[Epub] CrossRef - Thermal ablation for papillary thyroid microcarcinoma located in the isthmus: a study with 3 years of follow-up
Lin Zheng, Fang-yi Liu, Jie Yu, Zhi-gang Cheng, Xiao-ling Yu, Xiao-cong Dong, Zhi-yu Han, Ping Liang
Future Oncology.2022; 18(4): 471. CrossRef - Trends in the Management of Localized Papillary Thyroid Carcinoma in the United States (2000–2018)
Elisa Pasqual, Julie Ann Sosa, Yingxi Chen, Sara J. Schonfeld, Amy Berrington de González, Cari M. Kitahara
Thyroid.2022; 32(4): 397. CrossRef - Management of Low-Risk Thyroid Cancers: Is Active Surveillance a Valid Option? A Systematic Review of the Literature
Renato Patrone, Nunzio Velotti, Stefania Masone, Alessandra Conzo, Luigi Flagiello, Chiara Cacciatore, Marco Filardo, Vincenza Granata, Francesco Izzo, Domenico Testa, Stefano Avenia, Alessandro Sanguinetti, Andrea Polistena, Giovanni Conzo
Journal of Clinical Medicine.2021; 10(16): 3569. CrossRef - Cost-Effectiveness Analysis of Active Surveillance Compared to Early Surgery in Small Papillary Thyroid Cancer: A Systemic Review
Han-sang Baek, Chai-ho Jeong, Jeonghoon Ha, Ja-Seong Bae, Jeong-soo Kim, Dong-Jun Lim, Chul-Min Kim
Cancer Management and Research.2021; Volume 13: 6721. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef
- Active Surveillance for Low-Risk Thyroid Cancers: A Review of Current Practice Guidelines

- Clinical Study
- A Phase II Multi-Center, Non-Randomized, Parallel Group, Non-Inferiority Study to Compare the Efficacy of No Radioactive Iodine Remnant Ablation to Remnant Ablation Treatment in Low- to Intermediate-Risk of Papillary Thyroid Cancer: The MOREthyroid Trial Protocol
- Eun Kyung Lee, You Jin Lee, Young Joo Park, Jae Hoon Moon, Ka Hee Yi, Koon Soon Kim, Joo Hee Lee, Sun Wook Cho, Jungnam Joo, Yul Hwangbo, Sujeong Go, Do Joon Park
- Endocrinol Metab. 2020;35(3):571-577. Published online September 22, 2020
- DOI: https://doi.org/10.3803/EnM.2020.681
- 4,636 View
- 119 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
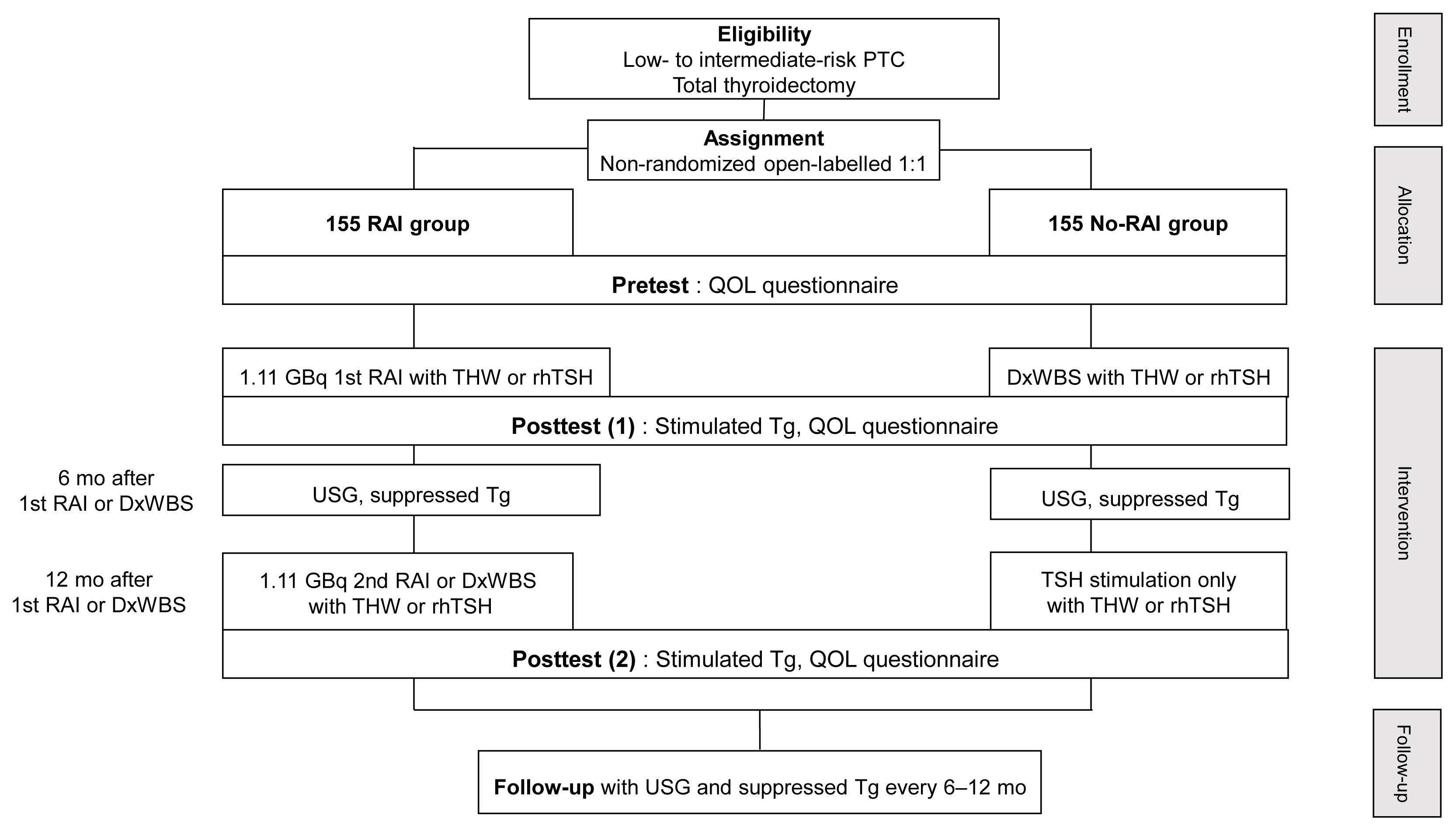
ePub - Background
Radioactive iodine (RAI) remnant ablation is recommended in patients with papillary thyroid cancer (PTC) and extrathyroidal extension or central lymph node metastasis. However, there exists little evidence about the necessity of remnant ablation in PTC patients with low- to intermediate-risk, those have been increasing in recent decades.
Methods
This multicenter, prospective, non-randomized, parallel group clinical trial will enroll 310 eligible patients with low- to intermediate-risk of thyroid cancer. Inclusion criteria are patients who recently underwent total thyroidectomy for PTC with 3 or less tumors of size 1≤ to ≤2 cm with no microscopic extension and N0/x, or size ≤2 cm with microscopic extension and/or N1a (number of lymph node ≤3, size of tumor foci ≤0.2 cm, and lymph node ratio <0.4). Patients choose to undergo RAI ablation (131I, dose 1.1 GBq) or diagnostic whole-body scan (DxWBS) (131I or 123I, dose 0.074 to 0.222 GBq), followed by subsequent measurement of stimulated thyroglobulin (sTg) within 1 year. Survey for quality of life (QOL) will be performed at baseline and at 1 year after follow-up. The total enrollment period is 5 years, and patients will be followed up for 1 year. The primary endpoint is the non-inferiority of surgery alone to surgery with ablation in terms of biochemical remission (BCR) rate (sTg ≤2 ng/mL) without evidence of structural recurrence. The secondary endpoint was the difference of QOL.
Conclusion
This study will evaluate whether surgery alone achieves similar BCR and improved QOL compared to RAI ablation in patients with low- to intermediate-risk PTC within 1 year.

- Clinical Study
- Subclinical Hypothyroidism Affects the Long-Term Outcomes of Patients Who Undergo Coronary Artery Bypass Grafting Surgery but Not Heart Valve Surgery
- Hana Kim, Sung Hye Kong, Jae Hoon Moon, Sang Yoon Kim, Kay-Hyun Park, Jun Sung Kim, Joong Haeng Choh, Young Joo Park, Cheong Lim
- Endocrinol Metab. 2020;35(2):308-318. Published online June 24, 2020
- DOI: https://doi.org/10.3803/EnM.2020.35.2.308
- 6,511 View
- 152 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
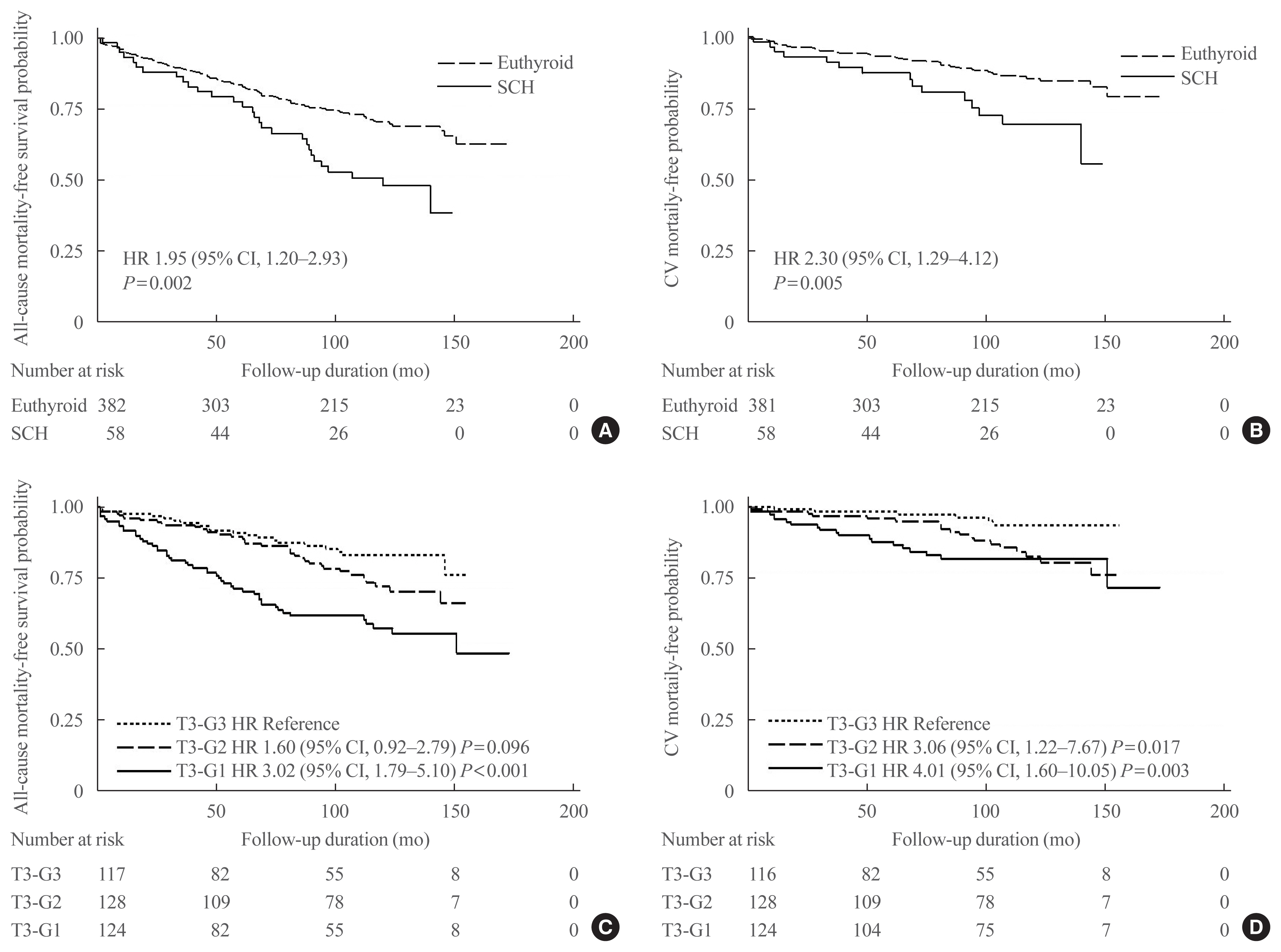
ePub - Background
The aim of this study was to determine the associations between subclinical hypothyroidism (SCH) and long-term cardiovascular outcomes after coronary artery bypass grafting (CABG) or heart valve surgery (HVS).
Methods
We retrospectively reviewed and compared all-cause mortality, cardiovascular mortality, and cardiovascular events in 461 patients who underwent CABG and 104 patients who underwent HVS.
Results
During a mean±standard deviation follow-up duration of 7.6±3.8 years, there were 187 all-cause deaths, 97 cardiovascular deaths, 127 major adverse cardiovascular events (MACE), 11 myocardial infarctions, one unstable angina, 70 strokes, 30 hospitalizations due to heart failure, 101 atrial fibrillation, and 33 coronary revascularizations. The incidence of all-cause mortality after CABG was significantly higher in patients with SCH (n=36, 55.4%) than in euthyroid patients (n=120, 30.3%), with a hazard ratio of 1.70 (95% confidence interval, 1.10 to 2.63; P=0.018) after adjustment for age, sex, current smoking status, body mass index, underlying diseases, left ventricular dysfunction, and emergency operation. Interestingly, low total triiodothyronine (T3) levels in euthyroid patients who underwent CABG were significantly associated with increased risks of all-cause mortality, cardiovascular mortality, and MACE, but those associations were not observed in HVS patients. Both free thyroxine and thyroid-stimulating hormone levels in euthyroid patients were not related with any cardiovascular outcomes in either the CABG or HVS group.
Conclusion
SCH or low total T3 might be associated with a poor prognosis after CABG, but not after HVS, implying that preoperative thyroid hormonal status may be important in ischemic heart disease patients. -
Citations
Citations to this article as recorded by- Subclinical hypothyroidism and clinical outcomes after cardiac surgery: A systematic review and meta-analysis
Michele Dell’Aquila, Camilla S. Rossi, Tulio Caldonazo, Gianmarco Cancelli, Lamia Harik, Giovanni J. Soletti, Kevin R. An, Jordan Leith, Hristo Kirov, Mudathir Ibrahim, Michelle Demetres, Arnaldo Dimagli, Mohamed Rahouma, Mario Gaudino
JTCVS Open.2024; 18: 64. CrossRef - The Association Between Hypothyroidism Treatment and Mortality in Patients Hospitalized in Surgical Wards
Hiba Masri-Iraqi, Yaron Rudman, Carmel Friedrich Dubinchik, Idit Dotan, Talia Diker-Cohen, Liat Sasson, Tzipora Shochat, Ilan Shimon, Eyal Robenshtok, Amit Akirov
Endocrine Research.2023; 48(2-3): 68. CrossRef - Mid-term outcomes of patients with subclinical hypothyroidism after coronary bypass surgery
Dong Zhao, Wei Zhao, Chuangshi Wang, Fei Xu, Wei Zhao, Xieraili Tiemuerniyazi, Hao Ma, Wei Feng
Interdisciplinary CardioVascular and Thoracic Surgery.2023;[Epub] CrossRef - Thyroid Pathology in High-Risk Cardiac Surgery Patients with Coronary Artery Disease
Olena K. Gogayeva, Anatoliy V. Rudenko, Vasyl V. Lazoryshynets, Serhii A. Rudenko, Tetiana A. Andrushchenko
Ukrainian Journal of Cardiovascular Surgery.2022; 30(1 (46)): 9. CrossRef - High-TSH Subclinical Hypothyroidism Is Associated With Postoperative Mortality in Acute Type A Aortic Dissection
Shi-Pan Wang, Yuan Xue, Hai-Yang Li, Wen-Jian Jiang, Hong-Jia Zhang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Triiodothyronine improves contractile recovery of human atrial trabeculae after hypoxia/reoxygenation
Petra Kleinbongard, Philipp Kuthan, Chantal Eickelmann, Philipp Jakobs, Joachim Altschmied, Judith Haendeler, Arjang Ruhparwar, Matthias Thielmann, Gerd Heusch
International Journal of Cardiology.2022; 363: 159. CrossRef - Hypothyroidism Is Correlated with Ventilator Complications and Longer Hospital Days after Coronary Artery Bypass Grafting Surgery in a Relatively Young Population: A Nationwide, Population-Based Study
Jiun-Yu Lin, Pei-Chi Kao, Yi-Ting Tsai, Chi-Hsiang Chung, Wu-Chien Chien, Chih-Yuan Lin, Chieh-Hua Lu, Chien-Sung Tsai
Journal of Clinical Medicine.2022; 11(13): 3881. CrossRef - Minor perturbations of thyroid homeostasis and major cardiovascular endpoints—Physiological mechanisms and clinical evidence
Patrick Müller, Melvin Khee-Shing Leow, Johannes W. Dietrich
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Subclinical Hypothyroidism: Prevalence, Health Impact, and Treatment Landscape
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2021; 36(3): 500. CrossRef
- Subclinical hypothyroidism and clinical outcomes after cardiac surgery: A systematic review and meta-analysis

- Thyroid
- Digital Medicine in Thyroidology: A New Era of Managing Thyroid Disease
- Jae Hoon Moon, Steven R. Steinhubl
- Endocrinol Metab. 2019;34(2):124-131. Published online June 24, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.2.124
- 5,399 View
- 135 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Digital medicine has the capacity to affect all aspects of medicine, including disease prediction, prevention, diagnosis, treatment, and post-treatment management. In the field of thyroidology, researchers are also investigating potential applications of digital technology for the thyroid disease. Recent studies using artificial intelligence (AI)/machine learning (ML) have reported reasonable performance for the classification of thyroid nodules based on ultrasonographic (US) images. AI/ML-based methods have also shown good diagnostic accuracy for distinguishing between benign and malignant thyroid lesions based on cytopathologic findings. Assistance from AI/ML methods could overcome the limitations of conventional thyroid US and fine-needle aspiration cytology. A web-based database has been developed for thyroid cancer care. In addition to its role as a nationwide registry of thyroid cancer, it is expected to serve as a clinical platform to facilitate better thyroid cancer care and as a research platform providing comprehensive disease-specific big data. Evidence has been found that biosignal monitoring with wearable devices may predict thyroid dysfunction. This real-world thyroid function monitoring could aid in the management and early detection of thyroid dysfunction. In the thyroidology field, research involving the range of digital medicine technologies and their clinical applications is expected to be even more active in the future.
-
Citations
Citations to this article as recorded by- AI in Thyroid Cancer Diagnosis: Techniques, Trends, and Future Directions
Yassine Habchi, Yassine Himeur, Hamza Kheddar, Abdelkrim Boukabou, Shadi Atalla, Ammar Chouchane, Abdelmalik Ouamane, Wathiq Mansoor
Systems.2023; 11(10): 519. CrossRef - Empirical Method for Thyroid Disease Classification Using a Machine Learning Approach
Tahir Alyas, Muhammad Hamid, Khalid Alissa, Tauqeer Faiz, Nadia Tabassum, Aqeel Ahmad, Gulnaz Afzal
BioMed Research International.2022; 2022: 1. CrossRef - Deep Learning Based Classification of Wrist Cracks from X-ray Imaging
Jahangir Jabbar, Muzammil Hussain, Hassaan Malik, Abdullah Gani, Ali Haider Khan, Muhammad Shiraz
Computers, Materials & Continua.2022; 73(1): 1827. CrossRef - Diagnostic Performance of Kwak, EU, ACR, and Korean TIRADS as Well as ATA Guidelines for the Ultrasound Risk Stratification of Non-Autonomously Functioning Thyroid Nodules in a Region with Long History of Iodine Deficiency: A German Multicenter Trial
Philipp Seifert, Simone Schenke, Michael Zimny, Alexander Stahl, Michael Grunert, Burkhard Klemenz, Martin Freesmeyer, Michael C. Kreissl, Ken Herrmann, Rainer Görges
Cancers.2021; 13(17): 4467. CrossRef - Association between Thyroid Function and Heart Rate Monitored by Wearable Devices in Patients with Hypothyroidism
Ki-Hun Kim, Juhui Lee, Chang Ho Ahn, Hyeong Won Yu, June Young Choi, Ho-Young Lee, Won Woo Lee, Jae Hoon Moon
Endocrinology and Metabolism.2021; 36(5): 1121. CrossRef - Deep Learning based Classification of Thyroid Cancer using Different Medical Imaging Modalities : A Systematic Review
Maheen Ilyas, Hassaan Malik, Muhammad Adnan, Umair Bashir, Wajahat Anwaar Bukhari, Muhammad Imran Ali Khan, Adnan Ahmad
VFAST Transactions on Software Engineering.2021; 9(4): 1. CrossRef - Ultrasound risk stratification systems for thyroid nodule: between lights and shadows, we are moving towards a new era
Pierpaolo Trimboli, Cosimo Durante
Endocrine.2020; 69(1): 1. CrossRef - Associations of Thyroid Hormones and Resting Heart Rate in Patients
Referred to Coronary Angiography
Eva Steinberger, Stefan Pilz, Christian Trummer, Verena Theiler-Schwetz, Markus Reichhartinger, Thomas Benninger, Marlene Pandis, Oliver Malle, Martin H. Keppel, Nicolas Verheyen, Martin R. Grübler, Jakob Voelkl, Andreas Meinitzer, Winfried März
Hormone and Metabolic Research.2020; 52(12): 850. CrossRef
- AI in Thyroid Cancer Diagnosis: Techniques, Trends, and Future Directions

- Miscellaneous
- Corrigendum: Author's Name Correction. Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-Jin Jeong, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun-Jae Chung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(3):427. Published online August 14, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.3.427
- 3,505 View
- 48 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population
Haytham Bayadsi, Martin Bergman, Malin Sund, Joakim Hennings
World Journal of Surgery.2020; 44(2): 461. CrossRef - Clinical and pathologic predictors of lymph node metastasis in papillary thyroid microcarcinomas
Ling Zhao, Xiaoya Sun, Yukun Luo, Fulin Wang, Zhaohui Lyu
Annals of Diagnostic Pathology.2020; 49: 151647. CrossRef
- Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population

- Thyroid
- Study Protocol of Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro)
- Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Kyu Eun Lee, Sung Hye Kong, Yeo Koon Kim, Woo-jin Jung, Chang Yoon Lee, Roh-Eul Yoo, Yul Hwangbo, Young Shin Song, Min Joo Kim, Sun Wook Cho, Su-jin Kim, Eun Jae Jung, June Young Choi, Chang Hwan Ryu, You Jin Lee, Jeong Hun Hah, Yuh-Seog Jung, Junsun Ryu, Yunji Hwang, Sue K. Park, Ho Kyung Sung, Ka Hee Yi, Do Joon Park, Young Joo Park
- Endocrinol Metab. 2018;33(2):278-286. Published online June 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.278
- 5,440 View
- 88 Download
- 34 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background The ongoing Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma (MAeSTro) aims to observe the natural course of papillary thyroid microcarcinoma (PTMC), develop a protocol for active surveillance (AS), and compare the long-term prognosis, quality of life, and medical costs between the AS and immediate surgery groups.
Methods This multicenter prospective cohort study of PTMC started in June 2016. The inclusion criteria were suspicious of malignancy or malignancy based on fine needle aspiration or core needle biopsy, age of ≥18 years, and a maximum diameter of ≤1 cm. If there was no major organ involvement, no lymph node/distant metastasis, and no variants with poor prognosis, the patients were explained of the pros and cons of immediate surgery and AS before selecting AS or immediate surgery. Follow-up visits (physical examination, ultrasonography, thyroid function, and questionnaires) are scheduled every 6 months during the first 2 years, and then every 1 year thereafter. Progression was defined as a maximum diameter increase of ≥3, ≥2 mm in two dimensions, suspected organ involvement, or lymph node/distant metastasis.
Results Among 439 enrolled patients, 290 patients (66.1%) chose AS and 149 patients (33.9%) chose immediate surgery. The median follow-up was 6.7 months (range, 0.2 to 11.9). The immediate surgery group had a larger maximum tumor diameter, compared to the AS group (7.1±1.9 mm vs. 6.6±2.0 mm, respectively;
P =0.014).Conclusion The results will be useful for developing an appropriate PTMC treatment policy based on its natural course and risk factors for progression.
-
Citations
Citations to this article as recorded by- 2023 Update of the Korean Thyroid Association Guidelines for the Management of Thyroid Nodules
Eun Kyung Lee, Young Joo Park
Clinical Thyroidology®.2024; 36(4): 153. CrossRef - Psychological adjustment to initial treatment for low‐risk thyroid cancer: Preliminary study
Gabriella T. Seo, Mark L. Urken, Lauren E. Wein, Michael P. Saturno, Danielle Kapustin, Monica H. Xing, Lauren E. Yue, Eric M. Dowling, Tracey A. Revenson, Katherine J. Roberts, Robert Michael Tuttle
Head & Neck.2023; 45(2): 439. CrossRef - Response to Letter to the Editor on Surgical Outcomes in Patients With Low-Risk Papillary Thyroid Microcarcinoma From MAeSTro Study: Immediate Operation Versus Delayed Operation Following Active Surveillance: A Multicenter Prospective Cohort Study
Hyeonuk Hwang, June Young Choi, Jae Hoon Moon, Eun Kyung Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jung
Annals of Surgery Open.2023; 4(3): e311. CrossRef - Lower Thyroid Cancer Mortality in Patients Detected by Screening: A Meta-Analysis
Shinje Moon, Young Shin Song, Kyong Yeun Jung, Eun Kyung Lee, Young Joo Park
Endocrinology and Metabolism.2023; 38(1): 93. CrossRef - To Screen or Not to Screen?
Do Joon Park
Endocrinology and Metabolism.2023; 38(1): 69. CrossRef - Surgical Outcomes in Patients With Low-risk Papillary Thyroid Microcarcinoma From MAeSTro Study
Hyeonuk Hwang, June Young Choi, Hyeong Won Yu, Jae Hoon Moon, Ji-hoon Kim, Eun Kyung Lee, Yeo Koon Kim, Chang Yoon Lee, Sun Wook Cho, Eun-Jae Chung, Chang Hwan Ryu, Junsun Ryu, Ka Hee Yi, Do Joon Park, Kyu Eun Lee, Young Joo Park, Su-jin Kim, Yuh-Seog Jun
Annals of Surgery.2023; 278(5): e1087. CrossRef - US Predictors of Papillary Thyroid Microcarcinoma Progression at Active Surveillance
Ji Ye Lee, Ji-hoon Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Jae Hoon Moon, Hoon Sung Choi, Hwangbo Yul, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Do Joon Park, Young Joo Park
Radiology.2023;[Epub] CrossRef - MET-receptor targeted fluorescent imaging and spectroscopy to detect multifocal papillary thyroid cancer
Madelon J. H. Metman, Pascal K. C. Jonker, Luc H. J. Sondorp, Bettien M. van Hemel, Mark S. Sywak, Anthony J. Gill, Liesbeth Jansen, Paul J. van Diest, Tessa M. van Ginhoven, Clemens W. G. M. Löwik, Anh H. Nguyen, Dominic J. Robinson, Gooitzen M. van Dam,
European Journal of Nuclear Medicine and Molecular Imaging.2023;[Epub] CrossRef - Active Surveillance of Thyroid Microcarcinomas: a Critical View
Claudio R. Cernea, Leandro Luongo Matos, Cecília Eugênio, Giovanna Mattos Ferreira, Yasmin Sa Cerqueira, Ana Kober N. Leite, Felipe A. B. Vanderlei, Dorival de Carlucci, Renato N. Gotoda, Flávio C. Hojaij, Vergilius J. F. Araújo-Filho
Current Oncology Reports.2022; 24(1): 69. CrossRef - Active Surveillance Versus Thyroid Surgery for Differentiated Thyroid Cancer: A Systematic Review
Roger Chou, Tracy Dana, Megan Haymart, Angela M. Leung, Ralph P. Tufano, Julie Ann Sosa, Matthew D. Ringel
Thyroid.2022; 32(4): 351. CrossRef - A Review of Active Surveillance of Papillary Thyroid Microcarcinoma
Cho Rok Lee
Journal of Endocrine Surgery.2022; 22(1): 1. CrossRef - Active Surveillance Versus Immediate Surgery for Low-Risk Papillary Thyroid Microcarcinoma Patients in South Korea: A Cost-Minimization Analysis from the MAeSTro Study
Kyungsik Kim, June Young Choi, Su-jin Kim, Eun Kyung Lee, Young Ki Lee, Jun Sun Ryu, Kyu Eun Lee, Jae Hoon Moon, Young Joo Park, Sun Wook Cho, Sue K. Park
Thyroid.2022; 32(6): 648. CrossRef - A cross-sectional survey of patient treatment choice in a multicenter prospective cohort study on active surveillance of papillary thyroid microcarcinoma (MAeSTro)
Yul Hwangbo, June Young Choi, Eun Kyung Lee, Chang Hwan Ryu, Sun Wook Cho, Eun Jae Chung, Jeong Hun Hah, Woo-Jin Jeong, Sue K. Park, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, You Jin Lee, Hyeong Won Yu,
Thyroid.2022;[Epub] CrossRef - Progression of Low-Risk Papillary Thyroid Microcarcinoma During Active Surveillance: Interim Analysis of a Multicenter Prospective Cohort Study of Active Surveillance on Papillary Thyroid Microcarcinoma in Korea
Eun Kyung Lee, Jae Hoon Moon, Yul Hwangbo, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Woo-Jin Jeong, Yuh-Seog Jung, Junsun Ryu, Su-jin Kim, Min Joo Kim, Yeo Koon Kim, Chang Yoon Lee, Ji Ye Lee, Hyeong Won Yu, Jeong Hun Hah, Kyu Eun Lee,
Thyroid.2022; 32(11): 1328. CrossRef - Indications and Strategy for Active Surveillance of Adult Low-Risk Papillary Thyroid Microcarcinoma: Consensus Statements from the Japan Association of Endocrine Surgery Task Force on Management for Papillary Thyroid Microcarcinoma
Iwao Sugitani, Yasuhiro Ito, Dai Takeuchi, Hirotaka Nakayama, Chie Masaki, Hisakazu Shindo, Masanori Teshima, Kazuhiko Horiguchi, Yusaku Yoshida, Toshiharu Kanai, Mitsuyoshi Hirokawa, Kiyomi Y. Hames, Isao Tabei, Akira Miyauchi
Thyroid.2021; 31(2): 183. CrossRef - Effect of Initial Treatment Choice on 2-year Quality of Life in Patients with Low-risk Papillary Thyroid Microcarcinoma
Jae Hoon Moon, Chang Hwan Ryu, Sun Wook Cho, June Young Choi, Eun-Jae Chung, Jeong Hun Hah, Yul Hwangbo, Woo-Jin Jeong, Yuh-Seog Jung, Ji-hoon Kim, Min Joo Kim, Su-jin Kim, Yeo Koon Kim, Chang Yoon Lee, Eun Kyung Lee, Ji Ye Lee, Kyu Eun Lee, You Jin Lee,
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): 724. CrossRef - Adoption of Active Surveillance for Very Low-Risk Differentiated Thyroid Cancer in the United States: A National Survey
Susan C Pitt, Nan Yang, Megan C Saucke, Nicholas Marka, Bret Hanlon, Kristin L Long, Alexandria D McDow, J P Brito, Benjamin R Roman
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): 1728. CrossRef - Protocol for a Korean Multicenter Prospective Cohort Study of Active Surveillance or Surgery (KoMPASS) in Papillary Thyroid Microcarcinoma
Min Ji Jeon, Yea Eun Kang, Jae Hoon Moon, Dong Jun Lim, Chang Yoon Lee, Yong Sang Lee, Sun Wook Kim, Min-Hee Kim, Bo Hyun Kim, Ho-Cheol Kang, Minho Shong, Sun Wook Cho, Won Bae Kim
Endocrinology and Metabolism.2021; 36(2): 359. CrossRef - Multifocality and Progression of Papillary Thyroid Microcarcinoma During Active Surveillance
Ryuta Nagaoka, Aya Ebina, Kazuhisa Toda, Tomoo Jikuzono, Marie Saitou, Masaomi Sen, Hiroko Kazusaka, Mami Matsui, Keiko Yamada, Hiroki Mitani, Iwao Sugitani
World Journal of Surgery.2021; 45(9): 2769. CrossRef - Active Surveillance as an Effective Management Option for Low-Risk Papillary Thyroid Microcarcinoma
Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2021; 36(4): 717. CrossRef - The Concept of Economic Evaluation and Its Application in Thyroid Cancer Research
Kyungsik Kim, Mijin Kim, Woojin Lim, Bo Hyun Kim, Sue K. Park
Endocrinology and Metabolism.2021; 36(4): 725. CrossRef - Genomic and Transcriptomic Characteristics According to Size of Papillary Thyroid Microcarcinoma
Young Shin Song, Byung-Hee Kang, Seungbok Lee, Seong-Keun Yoo, Young Sik Choi, Jungsun Park, Dong Yoon Park, Kyu Eun Lee, Jeong-Sun Seo, Young Joo Park
Cancers.2020; 12(5): 1345. CrossRef - Experience with Active Surveillance of Thyroid Low-Risk Carcinoma in a Developing Country
Alvaro Sanabria
Thyroid.2020; 30(7): 985. CrossRef - Association of Patient Age With Progression of Low-risk Papillary Thyroid Carcinoma Under Active Surveillance
Alexandra Koshkina, Rouhi Fazelzad, Iwao Sugitani, Akira Miyauchi, Lehana Thabane, David P. Goldstein, Sangeet Ghai, Anna M. Sawka
JAMA Otolaryngology–Head & Neck Surgery.2020; 146(6): 552. CrossRef - Active surveillance in low risk papillary thyroid carcinoma
Fabian Pitoia, Anabella Smulever
World Journal of Clinical Oncology.2020; 11(6): 320. CrossRef - Early Diagnosis of Low-Risk Papillary Thyroid Cancer Results Rather in Overtreatment Than a Better Survival
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Agnieszka Kotecka-Blicharz, Katarzyna Drosik-Rutowicz, Malgorzata Haras-Gil, Barbara Jarzab, Daria Handkiewicz-Junak
Frontiers in Endocrinology.2020;[Epub] CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición.2019; 66(8): 469. CrossRef - Computed Tomography for Detecting Cervical Lymph Node Metastasis in Patients Who Have Papillary Thyroid Microcarcinoma with Tumor Characteristics Appropriate for Active Surveillance
Dong-Hwa Lee, Yeo Koon Kim, Hyeong Won Yu, June Young Choi, So Yeon Park, Jae Hoon Moon
Thyroid.2019; 29(11): 1653. CrossRef - The dilemma of papillary thyroid microcarcinoma management. To operate or not to operate, that is the question
Juan C Galofré
Endocrinología, Diabetes y Nutrición (English ed.).2019; 66(8): 469. CrossRef - Longitudinal Assessment of Quality of Life According to Treatment Options in Low-Risk Papillary Thyroid Microcarcinoma Patients: Active Surveillance or Immediate Surgery (Interim Analysis of MAeSTro)
Sung Hye Kong, Junsun Ryu, Min Joo Kim, Sun Wook Cho, Young Shin Song, Ka Hee Yi, Do Joon Park, Yul Hwangbo, You Jin Lee, Kyu Eun Lee, Su-jin Kim, Woo-Jin Jeong, Eun-Jae Chung, Jeong Hun Hah, June Young Choi, Chang Hwan Ryu, Yuh-Seog Jung, Jae Hoon Moon,
Thyroid.2019; 29(8): 1089. CrossRef - Ultrasound-guided percutaneous laser ablation for papillary thyroid microcarcinoma: a retrospective analysis of 37 patients
Lili Ji, Qin Wu, Jun Gu, Xuedong Deng, Wei Zhou, Xing Fan, Feng Zhou
Cancer Imaging.2019;[Epub] CrossRef - Evolving management considerations in active surveillance for micropapillary thyroid carcinoma
Allen S. Ho, Irene Chen, Michelle Melany, Wendy L. Sacks
Current Opinion in Endocrinology, Diabetes & Obesity.2018; 25(5): 353. CrossRef
- 2023 Update of the Korean Thyroid Association Guidelines for the Management of Thyroid Nodules

- Thyroid
- Star-Shaped Intense Uptake of 131I on Whole Body Scans Can Reflect Good Therapeutic Effects of Low-Dose Radioactive Iodine Treatment of 1.1 GBq
- Sung Hye Kong, Jung Ah Lim, Young Shin Song, Shinje Moon, Ye An Kim, Min Joo Kim, Sun Wook Cho, Jae Hoon Moon, Ka Hee Yi, Do Joon Park, Bo Youn Cho, Young Joo Park
- Endocrinol Metab. 2018;33(2):228-235. Published online May 4, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.2.228
- 5,302 View
- 50 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background After initial radioactive iodine (RAI) treatment in differentiated thyroid cancer patients, we sometimes observe a star-shaped region of intense uptake of 131I on whole body scans (WBSs), called a ‘star artifact.’ We evaluated the clinical implications of star artifacts on the success rate of remnant ablation and long-term prognosis.
Methods Total 636 patients who received 131I dose of 1.1 GBq for the initial RAI therapy and who did not show distant metastasis at the time of diagnosis were retrospectively evaluated. A negative second WBS was used for evaluating the ablation efficacy of the RAI therapy. Among them, 235 patients (36.9%) showed a star artifact on their first WBS.
Results In patients with first stimulated thyroglobulin (sTg) levels ≤2 ng/mL, patients with star artifacts had a higher rate of negative second WBS compared with those without star artifacts (77.8% vs. 63.9%,
P =0.044), and showed significantly higher recurrence-free survival (P =0.043) during the median 8.0 years (range, 1.0 to 10.0) of follow-up. The 5- and 10-year recurrence rates (5YRR, 10YRR) were also significantly lower in patients with star artifacts compared with those without (0% vs. 4.9%, respectively,P =0.006 for 5YRR; 0% vs. 6.4%, respectively,P =0.005 for 10YRR). However, ablation success rate or recurrence-free survival was not different among patients whose first sTg levels >2 ng/mL regardless of star artifacts.Conclusion Therefore, star artifacts at initial RAI therapy imply a good ablation efficacy or a favorable long-term prognosis in patients with sTg levels ≤2 ng/mL.
-
Citations
Citations to this article as recorded by- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients
Liu Xiao, Wen Jie Zhang, Yue Qi Wang, Lin Li
Revista Española de Medicina Nuclear e Imagen Molecular (English Edition).2021; 40(1): 30. CrossRef - Valores pronósticos de la captación en estrella de 131I en pacientes con cáncer diferenciado de tiroides
L. Xiao, W.J. Zhang, Y.Q. Wang, L. Li
Revista Española de Medicina Nuclear e Imagen Molecular.2021; 40(1): 30. CrossRef - Comparison between planar and single-photon computed tomography images for radiation intensity quantification in iodine-131 scintigraphy
Yusuke Iizuka, Tomohiro Katagiri, Minoru Inoue, Kiyonao Nakamura, Takashi Mizowaki
Scientific Reports.2021;[Epub] CrossRef
- Prognostic value of star-shaped intense uptake of 131I in thyroid cancer patients

- Thyroid
- Validity and Reliability of the Korean Version of the Hyperthyroidism Symptom Scale
- Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
- Endocrinol Metab. 2018;33(1):70-78. Published online March 21, 2018
- DOI: https://doi.org/10.3803/EnM.2018.33.1.70
- 4,049 View
- 55 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Thyrotoxicosis is a common disease resulting from an excess of thyroid hormones, which affects many organ systems. The clinical symptoms and signs are relatively nonspecific and can vary depending on age, sex, comorbidities, and the duration and cause of the disease. Several symptom rating scales have been developed in an attempt to assess these symptoms objectively and have been applied to diagnosis or to evaluation of the response to treatment. The aim of this study was to assess the reliability and validity of the Korean version of the hyperthyroidism symptom scale (K-HSS).
Methods Twenty-eight thyrotoxic patients and 10 healthy subjects completed the K-HSS at baseline and after follow-up at Seoul National University Bundang Hospital. The correlation between K-HSS scores and thyroid function was analyzed. K-HSS scores were compared between baseline and follow-up in patient and control groups. Cronbach's α coefficient was calculated to demonstrate the internal consistency of K-HSS.
Results The mean age of the participants was 34.7±9.8 years and 13 (34.2%) were men. K-HSS scores demonstrated a significant positive correlation with serum free thyroxine concentration and decreased significantly with improved thyroid function. K-HSS scores were highest in subclinically thyrotoxic subjects, lower in patients who were euthyroid after treatment, and lowest in the control group at follow-up, but these differences were not significant. Cronbach's α coefficient for the K-HSS was 0.86.
Conclusion The K-HSS is a reliable and valid instrument for evaluating symptoms of thyrotoxicosis in Korean patients.
-
Citations
Citations to this article as recorded by- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)
Ja Kyung Lee, Eu Jeong Ku, Su-jin Kim, Woochul Kim, Jae Won Cho, Kyong Yeun Jung, Hyeong Won Yu, Yea Eun Kang, Mijin Kim, Hee Kyung Kim, Junsun Ryu, June Young Choi
Annals of Surgical Treatment and Research.2024; 106(1): 19. CrossRef - Effect of increased levothyroxine dose on depressive mood in older adults undergoing thyroid hormone replacement therapy
Jae Hoon Moon, Ji Won Han, Tae Jung Oh, Sung Hee Choi, Soo Lim, Ki Woong Kim, Hak Chul Jang
Clinical Endocrinology.2020; 93(2): 196. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef
- Effect of thyroid-stimulating hormone suppression on quality of life in thyroid lobectomy patients: interim analysis of a multicenter, randomized controlled trial in low- to intermediate-risk thyroid cancer patients (MASTER study)

- Endocrine Risk Factors for Cognitive Impairment
- Jae Hoon Moon
- Endocrinol Metab. 2016;31(2):185-192. Published online April 25, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.185
- 4,526 View
- 49 Download
- 22 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Cognitive impairment, including Alzheimer's disease and other kinds of dementia, is a major health problem in older adults worldwide. Although numerous investigators have attempted to develop effective treatment modalities or drugs, there is no reasonably efficacious strategy for preventing or recovering from cognitive impairment. Therefore, modifiable risk factors for cognitive impairment have received attention, and the growing literature of metabolic risk factors for cognitive impairment has expanded from epidemiology to molecular pathogenesis and therapeutic management. This review focuses on the epidemiological evidence for the association between cognitive impairment and several endocrine risk factors, including insulin resistance, dyslipidemia, thyroid dysfunction, vitamin D deficiency, and subclinical atherosclerosis. Researches suggesting possible mechanisms for this association are reviewed. The research investigating modifiable endocrine risk factors for cognitive impairment provides clues for understanding the pathogenesis of cognitive impairment and developing novel treatment modalities. However, so far, interventional studies investigating the beneficial effect of the "modification" of these "modifiable risk factors" on cognitive impairment have reported variable results. Therefore, well-designed, randomized prospective interventional studies are needed.
-
Citations
Citations to this article as recorded by- Association between the neutrophil to lymphocyte ratio and mild cognitive impairment in patients with type 2 diabetes
Zi-Wei Yu, Ying Wang, Xin Li, Xue-Wei Tong, Yi-Tong Zhang, Xin-Yuan Gao
Aging Clinical and Experimental Research.2023; 35(6): 1339. CrossRef - Cognitive status and its risk factors in patients with hypertension and diabetes in a low‐income rural area of China: A cross‐sectional study
Yuyan Guo, Ruifeng Liang, Jingjuan Ren, Liting Cheng, Mengqin Wang, Huilin Chai, Xiaoyu Cheng, Yaowen Yang, Yajuan Sun, Jiantao Li, Shuhong Zhao, Wenjing Hou, Jianhua Zhang, Feng Liu, Rong Wang, Qiao Niu, Hongmei Yu, Shoulin Yang, Jianying Bai, Hongmei Zh
International Journal of Geriatric Psychiatry.2023;[Epub] CrossRef - Insulin Resistance and Glucose Metabolism during Infection
Borros Arneth
Endocrines.2023; 4(4): 685. CrossRef - Corresponding risk factors between cognitive impairment and type 1 diabetes mellitus: A narrative review
Chen-Yang Jin, Shi-Wen Yu, Jun-Ting Yin, Xiao-Ying Yuan, Xu-Gang Wang
Heliyon.2022; 8(8): e10073. CrossRef - Cerebrospinal fluid heart fatty acid‐binding protein as a predictive biomarker of neurodegeneration in Alzheimer’s disease
Lu Pan, Ya-Nan Ou, Lin Tan, Lan Tan, Jin-Tai Yu
Brain Science Advances.2021; 7(1): 44. CrossRef - Endocrine dysfunction and cognitive impairment
Valeria CALSOLARO, Marina BOTTARI, Giulia COPPINI, Bianca LEMMI, Fabio MONZANI
Minerva Endocrinology.2021;[Epub] CrossRef - Effect of hypothyroidism on cognitive status: Evidence from stroop task
Shilpi Goyal, Abhinav Dixit, Neelam Vaney, SV Madhu
Indian Journal of Medical Specialities.2020; 11(1): 34. CrossRef - Statin use and safety concerns: an overview of the past, present, and the future
Rubina Mulchandani, Tanica Lyngdoh, Ashish Kumar Kakkar
Expert Opinion on Drug Safety.2020; 19(8): 1011. CrossRef - Neurocognitive impairment in type 2 diabetes mellitus
Marianna Karvani, P. Simos, S. Stavrakaki, D. Kapoukranidou
Hormones.2019; 18(4): 523. CrossRef - TDP-43 proteinopathy in aging: Associations with risk-associated gene variants and with brain parenchymal thyroid hormone levels
Peter T. Nelson, Zsombor Gal, Wang-Xia Wang, Dana M. Niedowicz, Sergey C. Artiushin, Samuel Wycoff, Angela Wei, Gregory A. Jicha, David W. Fardo
Neurobiology of Disease.2019; 125: 67. CrossRef - Treated hypothyroidism is associated with cerebrovascular disease but not Alzheimer's disease pathology in older adults
Willa D. Brenowitz, Fang Han, Walter A. Kukull, Peter T. Nelson
Neurobiology of Aging.2018; 62: 64. CrossRef - Translating molecular advances in Down syndrome and Fragile X syndrome into therapies
Victor Faundez, Ilario De Toma, Barbara Bardoni, Renata Bartesaghi, Dean Nizetic, Rafael de la Torre, Roi Cohen Kadosh, Yann Herault, Mara Dierssen, Marie-Claude Potier, Stylianos Antonarakis, Renata Bartesaghi, Andrea Contestabile, Tonnie Coppus, Peter D
European Neuropsychopharmacology.2018; 28(6): 675. CrossRef - Associations between waist circumference, metabolic risk and executive function in adolescents: A cross-sectional mediation analysis
Anna Bugge, Sören Möller, Daniel R. Westfall, Jakob Tarp, Anne K. Gejl, Niels Wedderkopp, Charles H. Hillman, Ying-Mei Feng
PLOS ONE.2018; 13(6): e0199281. CrossRef - BsmI polymorphism in the vitamin D receptor gene is associated with 25-hydroxy vitamin D levels in individuals with cognitive decline
Ana Carolina R. de Oliveira, Carolina A. Magalhães, Cristina M. G. Loures, Vanessa G. Fraga, Leonardo C. de Souza, Henrique C. Guimarães, Marco T. G. Cintra, Maria A. Bicalho, Maira C. R. Sousa, Josianne N. Silveira, Ieda F. O. Silva, Paulo Caramelli, Mar
Arquivos de Neuro-Psiquiatria.2018; 76(11): 760. CrossRef - Traumatic brain injury: sex, gender and intersecting vulnerabilities
Tatyana Mollayeva, Shirin Mollayeva, Angela Colantonio
Nature Reviews Neurology.2018; 14(12): 711. CrossRef - Determinants of poor cognitive function using A-IQCODE among Lebanese older adults: a cross-sectional study
Ibrahim R. Bou-Orm, Assem M. Khamis, Monique Chaaya
Aging & Mental Health.2018; 22(6): 844. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - Alcohol consumption and gastric cancer risk: a meta-analysis of prospective cohort studies
Xue Han, Li Xiao, Yao Yu, Yu Chen, Hai-Hua Shu
Oncotarget.2017; 8(47): 83237. CrossRef - Functional capacity and obesity reflect the cognitive performance of older adults living in long‐term care facilities
Karine Gonçalves Damascena, Cristiane Batisti Ferreira, Pâmela dos Santos Teixeira, Bibiano Madrid, Alexandre Gonçalves, Cláudio Córdova, Otávio de Toledo Nóbrega, Aparecido Pimentel Ferreira
Psychogeriatrics.2017; 17(6): 439. CrossRef - Insulin resistance, dyslipidemia, and apolipoprotein E interactions as mechanisms in cognitive impairment and Alzheimer's disease
Therese S Salameh, Elizabeth M Rhea, William A Banks, Angela J Hanson
Experimental Biology and Medicine.2016; 241(15): 1676. CrossRef - Role of the Orexin System on the Hypothalamus-Pituitary-Thyroid Axis
Antonietta Messina, Carolina De Fusco, Vincenzo Monda, Maria Esposito, Fiorenzo Moscatelli, Anna Valenzano, Marco Carotenuto, Emanuela Viggiano, Sergio Chieffi, Vincenzo De Luca, Giuseppe Cibelli, Marcellino Monda, Giovanni Messina
Frontiers in Neural Circuits.2016;[Epub] CrossRef - Genomics and CSF analyses implicate thyroid hormone in hippocampal sclerosis of aging
Peter T. Nelson, Yuriko Katsumata, Kwangsik Nho, Sergey C. Artiushin, Gregory A. Jicha, Wang-Xia Wang, Erin L. Abner, Andrew J. Saykin, Walter A. Kukull, David W. Fardo
Acta Neuropathologica.2016; 132(6): 841. CrossRef
- Association between the neutrophil to lymphocyte ratio and mild cognitive impairment in patients with type 2 diabetes

- Clinical Study
- Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011
- Dong-Hwa Lee, Kyong Yeun Jung, Kyeong Seon Park, Kyoung Min Kim, Jae Hoon Moon, Soo Lim, Hak Chul Jang, Sung Hee Choi
- Endocrinol Metab. 2015;30(4):514-521. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.514
- 3,601 View
- 42 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The present study aimed to investigate the clinical characteristics of type 2 diabetes mellitus (T2DM) in Korean adults according to body mass index (BMI) and to analyze the association with cardiovascular disease (CVD).
Methods We conducted a cross-sectional study of data from the Korea National Health and Nutrition Examination Survey from 2007 to 2011. A total of 3,370 patients with T2DM were divided into categories according to BMI. We conducted a comparison of the T2DM patient population composition by BMI category between different countries. We investigated the prevalence of awareness, treatment, and target control of T2DM according to BMI.
Results Patients with T2DM had a higher BMI, and were more likely to have a history of CVD than healthy controls. For Korean adults with T2DM, 8% had BMI ≥30 kg/m2. By contrast, the population of patients with T2DM and BMI ≥30 kg/m2 was 72% in patients in the USA and 56% in the UK. The rate of recognition, treatment, and control has worsened in parallel with increasing BMI. Even in patients with BMI 25 to 29.9 kg/m2, the prevalence of CVD or high risk factors for CVD was significantly higher than in patients with BMI 18.5 to 22.9 kg/m2 (odds ratio, 2.07).
Conclusion Korean patients with T2DM had lower BMI than those in Western countries. Higher BMI was associated with lower awareness, treatment, and control of diabetes, and a positive association was observed between CVD or high risk factors for CVD and BMI, even for patients who were overweight but not obese.
-
Citations
Citations to this article as recorded by- Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diet Quality Scores and Asthenoteratozoospermia Risk: Finding From a Hospital-Based Case–Control Study in China
Qi Cui, Hui-Han Wang, Qi-Jun Wu, Xiao-Bin Wang, Ren-Hao Guo, Xu Leng, Xiao-Ling Tan, Qiang Du, Bo-Chen Pan
Frontiers in Nutrition.2022;[Epub] CrossRef - Obesity definition for personalised treatment of type 2 diabetes Authors’ reply
Ildiko Lingvay, Priya Sumithran, Ricardo V Cohen, Carel W le Roux
The Lancet.2022; 399(10342): 2189. CrossRef - Secular trends and determinants of influenza vaccination uptake among patients with cardiovascular disease in Korea: Analysis using a nationwide database
Min Kim, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, So Rae Kim, Kyeong Seok Oh, Woong-Su Yoon, Dae-Hwan Bae, Ju Hee Lee, Sang Min Kim, Woong Gil Choi, Jang-Whan Bae, Kyung-Kuk Hwang, Dong-Woon Kim, Myeong-Chan Cho, Hyun Lee, Dae-In Lee
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Triglyceride glucose (TyG) index as a predictor of incident type 2 diabetes among nonobese adults: a 12-year longitudinal study of the Korean Genome and Epidemiology Study cohort
Byoungjin Park, Hye Sun Lee, Yong-Jae Lee
Translational Research.2021; 228: 42. CrossRef - Gamitaeeumjowee-Tang for weight loss in diabetic patients: A retrospective chart review
A-Reum Lee, Da-Yeon Lee, Min-Ji Kim, Hyang-Sook Lee, Ka-Hye Choi, Seo-Young Kim, Young-Woo Lim, Young-Bae Park
Journal of Korean Medicine.2021; 42(1): 46. CrossRef - Effect of cilostazol, a phosphodiesterase‐3 inhibitor, on coronary artery stenosis and plaque characteristics in patients with type 2 diabetes: ESCAPE study
Dong‐Hwa Lee, Eun Ju Chun, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Hak Chul Jang, Soo Lim
Diabetes, Obesity and Metabolism.2019; 21(6): 1409. CrossRef - The Differential Role of Vitamin D in Type 2 Diabetes Management and Control in Minority Populations
Miyong To Kim, Kim Byeng Kim, Jisook Ko, Nicole Murry, David Levine, Ju-Young Lee
Journal of Immigrant and Minority Health.2019; 21(6): 1266. CrossRef - House dust mite and Cockroach specific Immunoglobulin E sensitization is associated with diabetes mellitus in the adult Korean population
Mee Kyoung Kim, Jee Sun Jeong, Kyungdo Han, Ki Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Scientific Reports.2018;[Epub] CrossRef - Long‐term effects on glycaemic control and β‐cell preservation of early intensive treatment in patients with newly diagnosed type 2 diabetes: A multicentre randomized trial
Suk Chon, Sang Youl Rhee, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Soon Jib Yoo, Gwanpyo Koh, Dae Ho Lee, Young Seol Kim, Jeong‐Taek Woo
Diabetes, Obesity and Metabolism.2018; 20(5): 1121. CrossRef - Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
Kyung Min Ko, Kyungdo Han, Youn Jee Chung, Kun-Ho Yoon, Yong Gyu Park, Seung-Hwan Lee
Endocrinology and Metabolism.2017; 32(2): 248. CrossRef - Abnormal subchondral bone remodeling and its association with articular cartilage degradation in knees of type 2 diabetes patients
Yan Chen, Yong-Can Huang, Chun Hoi Yan, Kwong Yuen Chiu, Qingjun Wei, Jingmin Zhao, X Edward Guo, Frankie Leung, William W Lu
Bone Research.2017;[Epub] CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Pharmacological Management of Obesity in Patients with Type 2 Diabetes: An Update
Eun Ju Lee, Tae Nyun Kim
The Korean Journal of Obesity.2016; 25(3): 121. CrossRef - Response: Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011 (Endocrinol Metab 2015;30:514-21, Dong-Hwa Lee et al.)
Sung Hee Choi
Endocrinology and Metabolism.2016; 31(2): 347. CrossRef - Letter: Characterization of Patients with Type 2 Diabetes according to Body Mass Index: Korea National Health and Nutrition Examination Survey from 2007 to 2011 (Endocrinol Metab 2015;30:514-21, Dong-Hwa Lee et al.)
Eun-Hee Cho
Endocrinology and Metabolism.2016; 31(2): 345. CrossRef
- Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database

- Thyroid
- The Diagnosis and Management of Hyperthyroidism in Korea: Consensus Report of the Korean Thyroid Association
- Jae Hoon Moon, Ka Hee Yi
- Endocrinol Metab. 2013;28(4):275-279. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.275
- 5,346 View
- 70 Download
- 54 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Hyperthyroidism is one of the causes of thyrotoxicosis and the most common cause of hyperthyroidism in Korea is Graves disease. The diagnosis and treatment of Graves disease are different according to geographical area. Recently, the American Thyroid Association and the American Association of Clinical Endocrinologists suggested new management guidelines for hyperthyroidism. However, these guidelines are different from clinical practice in Korea and are difficult to apply. Therefore, the Korean Thyroid Association (KTA) conducted a survey of KTA members regarding the diagnosis and treatment of hyperthyroidism, and reported the consensus on the management of hyperthyroidism. In this review, we summarized the KTA report on the contemporary practice patterns in the diagnosis and management of hyperthyroidism, and compared this report with guidelines from other countries.
-
Citations
Citations to this article as recorded by- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas
Mika Tamura, Kunihiro Nakada, Haruna Iwanaga, Naotoshi Fujita, Katsuhiko Kato
European Journal of Nuclear Medicine and Molecular Imaging.2024; 51(4): 1060. CrossRef - Effects of altitude on thyroid disorders according to Chinese three-rung, ladder-like topography: national cross-sectional study
Boshen Gong, Youmin Wang, Jin-an Zhang, Qiao Zhang, Jiajun Zhao, Jiashu Li, Xichang Wang, Yutong Han, Ziwei Yu, Chenyu Zhang, Bingcong Peng, Yumin Xing, Qiuxian Li, Ping Wang, Yongze Li, Weiping Teng, Zhongyan Shan
BMC Public Health.2024;[Epub] CrossRef - MACE and Hyperthyroidism Treated With Medication, Radioactive Iodine, or Thyroidectomy
Carol Chiung-Hui Peng, Yu-Jie Lin, Sun Y. Lee, Shu-Man Lin, Cheng Han, Ching-Hui Loh, Huei-Kai Huang, Elizabeth N. Pearce
JAMA Network Open.2024; 7(3): e240904. CrossRef - Increased risk of incident gout in patients with hyperthyroidism: a nationwide retrospective cohort study
Ju-Yeun Lee, So-Yeon Park, Seo Young Sohn
Rheumatology International.2023; 44(3): 451. CrossRef - The Current Status of Hyperthyroidism in Korea
Hyemi Kwon
Endocrinology and Metabolism.2023; 38(4): 392. CrossRef - A machine learning-assisted system to predict thyrotoxicosis using patients’ heart rate monitoring data: a retrospective cohort study
Kyubo Shin, Jongchan Kim, Jaemin Park, Tae Jung Oh, Sung Hye Kong, Chang Ho Ahn, Joon Ho Moon, Min Joo Kim, Jae Hoon Moon
Scientific Reports.2023;[Epub] CrossRef - Immunometabolic signatures predict recovery from thyrotoxic myopathy in patients with Graves' disease
Daiki Setoyama, Ho Yeop Lee, Ji Sun Moon, Jingwen Tian, Yea Eun Kang, Ju Hee Lee, Minho Shong, Dongchon Kang, Hyon‐Seung Yi
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(1): 355. CrossRef - Comparison of 99mTc Pertechnetate Thyroid Uptake Rates by Gamma Probe and Gamma Camera Methods for Differentiating Graves’ Disease and Thyroiditis
Meihua Jin, Jonghwa Ahn, Seong-gil Jo, Jangwon Park, Min Ji Jeon, Won Gu Kim, Tae Yong Kim, Won Bae Kim, Young Kee Shong, Jin-Sook Ryu
Nuclear Medicine and Molecular Imaging.2022; 56(1): 42. CrossRef - KSNM60 in Nuclear Endocrinology: from the Beginning to the Future
Chae Moon Hong, Young Jin Jeong, Hae Won Kim, Byeong-Cheol Ahn
Nuclear Medicine and Molecular Imaging.2022; 56(1): 17. CrossRef - Graves’ disease and the risk of Parkinson’s disease: a Korean population-based study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Jinyoung Youn, Ji Oh Mok, Chul-Hee Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Brain Communications.2022;[Epub] CrossRef - Graves’ Disease and the Risk of End-Stage Renal Disease: A Korean Population-Based Study
Yoon Young Cho, Bongseong Kim, Dong Wook Shin, Hye Ryoun Jang, Bo-Yeon Kim, Chan-Hee Jung, Jae Hyeon Kim, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Endocrinology and Metabolism.2022; 37(2): 281. CrossRef - Evaluation and Management of Bone Health in Patients with Thyroid Diseases: a Position Statement from the Korean Thyroid Association
A Ram Hong, Hwa Young Ahn, Bu Kyung Kim, Seong Hee Ahn, So Young Park, Min-Hee Kim, Jeongmin Lee, Sun Wook Cho, Ho-Cheol Kang
International Journal of Thyroidology.2022; 15(1): 1. CrossRef - Patient Population and Test Utilization for Thyroid Function in Local Clinics and Hospitals in Korea
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Diagnostics.2022; 12(7): 1638. CrossRef - 2021 Asia-Pacific Graves’ Disease Consortium Survey of Clinical Practice Patterns in the Management of Graves’ Disease
Rajeev Parameswaran, Mechteld Christine de Jong, James Lee Wai Kit, Kathleen Sek, Tran Quang Nam, Tran Viet Thang, Nguyen Thy Khue, Than Than Aye, Phone Myint Tun, Timothy Cole, Julie A. Miller, Michael Villa, Benjapa Khiewvan, Sirinart Sirinvaravong, Yon
Endocrine.2022; 79(1): 135. CrossRef - Graves’ disease, its treatments, and the risk of atrial fibrillation: A Korean population-based study
Yoon Young Cho, Bongseong Kim, Dughyun Choi, Chul-Hee Kim, Dong Wook Shin, Jee Soo Kim, Seung-Jung Park, Sun Wook Kim, Jae Hoon Chung, Kyungdo Han, Tae Hyuk Kim
Frontiers in Endocrinology.2022;[Epub] CrossRef - Forty Years Together, New Leap Forward! The 40th Anniversary of the Korean Endocrine Society
Jong Chul Won, Ki-Hyun Baek
Endocrinology and Metabolism.2022; 37(6): 851. CrossRef - Evaluation of the role of thyroid scintigraphy in the differential diagnosis of thyrotoxicosis
Carolina M. Perdomo, Marta García‐Goñi, Lidia Sancho, José J. Paricio, María D. Lozano, Magdalena de la Higuera, María Currás, Javier Arbizu, Juan C. Galofré
Clinical Endocrinology.2021; 94(3): 466. CrossRef - Treatment of patients with Graves’ disease in Sweden compared to international surveys of an ‘index patient’
Gabriel Sjölin, Kristina Byström, Mats Holmberg, Ove Törring, Selwan Khamisi, Jan Calissendorff, Mikael Lantz, Bengt Hallengren, Helena Filipsson Nyström, Tereza Planck, Göran Wallin
Endocrinology, Diabetes & Metabolism.2021;[Epub] CrossRef - Secular Trends in Ablation Therapy for Graves’ Disease: An Analysis of a 15-Year Experience at a Tertiary Hospital in South Korea
Min Joo Kim, Ye An Kim, Sun Wook Cho, Su-jin Kim, Kyu Eun Lee, Young Joo Park, Do Joon Park, Bo Youn Cho
Journal of Clinical Medicine.2021; 10(8): 1629. CrossRef - Long-Term Antithyroid Drug Treatment of Graves’ Disease in Children and Adolescents: A 20-Year Single-Center Experience
Ari Song, Su Jin Kim, Min-Sun Kim, Jiyeon Kim, Insung Kim, Ga Young Bae, Eunseop Seo, Young Seok Cho, Joon Young Choi, Sung Yoon Cho, Dong-Kyu Jin
Frontiers in Endocrinology.2021;[Epub] CrossRef - Association of Polygenetic Risk Scores Related to Immunity and Inflammation with Hyperthyroidism Risk and Interactions between the Polygenetic Scores and Dietary Factors in a Large Cohort
Mi Young Song, Sunmin Park, Anjali Mishra
Journal of Thyroid Research.2021; 2021: 1. CrossRef - Treatment Modality and Risk of Heart Failure in Patients With Long-Standing Graves’ Disease: A Nationwide Population-Based Cohort Study
Eyun Song, Mina Kim, Sojeong Park, Min Jeong Park, Jung A. Kim, Eun Roh, Ji Hee Yu, Nam Hoon Kim, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Frontiers in Endocrinology.2021;[Epub] CrossRef - Risk of Diabetes in Patients with Long-Standing Graves’ Disease: A Longitudinal Study
Eyun Song, Min Ji Koo, Eunjin Noh, Soon Young Hwang, Min Jeong Park, Jung A Kim, Eun Roh, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
Endocrinology and Metabolism.2021; 36(6): 1277. CrossRef - Diabetes and Hyperthyroidism: Is There a Causal Link?
Sang Yong Kim
Endocrinology and Metabolism.2021; 36(6): 1175. CrossRef - Incidence and Mortality of Myocardial Infarction and Stroke in Patients with Hyperthyroidism: A Nationwide Cohort Study in Korea
Hyun Jung Kim, Taeuk Kang, Min Ji Kang, Hyeong Sik Ahn, Seo Young Sohn
Thyroid.2020; 30(7): 955. CrossRef - Diagnosis and Management of Graves’ Disease in Thailand: A Survey of Current Practice
Chutintorn Sriphrapradang
Journal of Thyroid Research.2020; 2020: 1. CrossRef - The success rate of radioactive iodine therapy for Graves’ disease in iodine-replete area and affecting factors: a single-center study
Hyunju Park, Hye In Kim, Jun Park, So Young Park, Tae Hyuk Kim, Jae Hoon Chung, Joon Young Choi, Sun Wook Kim
Nuclear Medicine Communications.2020; 41(3): 212. CrossRef - Tirotoksikoz nedenli erektil disfonksiyon üzerine sildenafil etkisinin histopatolojik olarak değerlendirilmesi
Murat ÖZDEMİR, Canberk TOMRUK, Gürkan YİĞİTTÜRK, Varlık EROL, Emel Öykü ÇETİN, Ilgın YILDIRIM ŞİMŞİR, Çiğdem YENİSEY, Yiğit UYANIKGİL, Adnan ŞİMŞİR, Özer MAKAY
Ege Tıp Dergisi.2020; 59(3): 215. CrossRef - The Management of Thyroid Disease in COVID-19 Pandemic
Won Sang Yoo, Hyun-Kyung Chung
International Journal of Thyroidology.2020; 13(2): 65. CrossRef - Is Hyperthyroidism Diagnosed and Treated Appropriately in the United States?
Ammar Asban, Sophie Dream, Brenessa Lindeman
Advances in Surgery.2019; 53: 117. CrossRef - Long-term remission following antithyroid drug withdrawal in patients with Graves’ hyperthyroidism: parameters with prognostic value
Ricardo V. García-Mayor, Paula Álvarez-Vázquez, Enrique Fluiters, Diana Valverde, Amalia Andrade
Endocrine.2019; 63(2): 316. CrossRef - Safety of long-term antithyroid drug treatment? A systematic review
F. Azizi, R. Malboosbaf
Journal of Endocrinological Investigation.2019; 42(11): 1273. CrossRef - Changes in Thyroid Peroxidase and Thyroglobulin Antibodies Might Be Associated with Graves' Disease Relapse after Antithyroid Drug Therapy
Yun Mi Choi, Mi Kyung Kwak, Sang Mo Hong, Eun-Gyoung Hong
Endocrinology and Metabolism.2019; 34(3): 268. CrossRef - Prevalence and Annual Incidence of Thyroid Disease in Korea from 2006 to 2015: A Nationwide Population-Based Cohort Study
Hyemi Kwon, Jin-hyung Jung, Kyung-Do Han, Yong-Gyu Park, Jung-Hwan Cho, Da Young Lee, Ji Min Han, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2018; 33(2): 260. CrossRef - An update in the treatment preference for hyperthyroidism
Obin Kwon
Nature Reviews Endocrinology.2018; 14(7): 438. CrossRef - Clinical Feasibility of Monitoring Resting Heart Rate Using a Wearable Activity Tracker in Patients With Thyrotoxicosis: Prospective Longitudinal Observational Study
Jie-Eun Lee, Dong Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Sung Hee Choi, Soo Lim, Young Joo Park, Do Joon Park, Hak Chul Jang, Jae Hoon Moon
JMIR mHealth and uHealth.2018; 6(7): e159. CrossRef - Graves' Disease Patients with Large Goiters Respond Best to Radioactive Iodine Doses of at Least 15 mCi: a Sonographic Volumetric Study
Yun Ah Jeong, Jee Hee Yoon, Hee Kyung Kim, Ho-Cheol Kang
International Journal of Thyroidology.2018; 11(2): 137. CrossRef - Chylothorax Associated with Substernal Goiter in Graves’ Disease Treated with Radioactive Iodine
Seo Young Oh, Bo Hyun Kim, Do Young Kim, Kyu Min Lee, Min Jin Lee, Sung Su Kim, Jong Ho Kim, Yun Kyung Jeon, Sang Soo Kim, Yong Ki Kim, In Joo Kim
International Journal of Endocrinology and Metabolism.2017;[Epub] CrossRef - Vitiligo and overt thyroid diseases: A nationwide population-based study in Korea
Jung Min Bae, June Hyunkyung Lee, Jae Seung Yun, Byeol Han, Tae Young Han
Journal of the American Academy of Dermatology.2017; 76(5): 871. CrossRef - Increased risk of thyroid diseases in patients with systemic lupus erythematosus: A nationwide population-based Study in Korea
Jae-Seung Yun, Jung Min Bae, Ki-Jo Kim, Yu Seok Jung, Gyong Moon Kim, Hyung-Rae Kim, Jun-Seok Lee, Seung-Hyun Ko, Seon-Ah Cha, Yu-Bae Ahn, Ludmila Prokunina-Olsson
PLOS ONE.2017; 12(6): e0179088. CrossRef - The Second Antithyroid Drug Treatment Is Effective in Relapsed Graves' Disease Patients: A Median 11-Year Follow-Up Study
Ye An Kim, Sun Wook Cho, Hoon Sung Choi, Shinje Moon, Jae Hoon Moon, Kyung Won Kim, Do Joon Park, Ka Hee Yi, Young Joo Park, Bo Youn Cho
Thyroid.2017; 27(4): 491. CrossRef - Free Thyroxine, Anti-Thyroid Stimulating Hormone Receptor Antibody Titers, and Absence of Goiter Were Associated with Responsiveness to Methimazole in Patients with New Onset Graves' Disease
Hoon Sung Choi, Won Sang Yoo
Endocrinology and Metabolism.2017; 32(2): 281. CrossRef - Long-Term Antithyroid Drug Treatment: A Systematic Review and Meta-Analysis
Fereidoun Azizi, Ramin Malboosbaf
Thyroid.2017; 27(10): 1223. CrossRef - The Recurrence Rate of Graves' Disease among Patients with Subclinical Thyrotoxicosis after Initial Remission with Antithyroid Agents
Myoung Sook Shim, Soo Min Nam, Jin Sae Yoo, Hae Kyung Kim, Sang Jun Lee, Mi Young Lee
International Journal of Thyroidology.2017; 10(2): 77. CrossRef - Serum 25-hydroxyvitamin D might be an independent prognostic factor for Graves disease recurrence
Hwa Young Ahn, Yun Jae Chung, Bo Youn Cho
Medicine.2017; 96(31): e7700. CrossRef - Recent Advances in Autoimmune Thyroid Diseases
Won Sang Yoo, Hyun Kyung Chung
Endocrinology and Metabolism.2016; 31(3): 379. CrossRef - Usefulness of Measuring Thyroid Stimulating Antibody at the Time of Antithyroid Drug Withdrawal for Predicting Relapse of Graves Disease
Hyemi Kwon, Won Gu Kim, Eun Kyung Jang, Mijin Kim, Suyeon Park, Min Ji Jeon, Tae Yong Kim, Jin-Sook Ryu, Young Kee Shong, Won Bae Kim
Endocrinology and Metabolism.2016; 31(2): 300. CrossRef - Hyperthyroidism
Simone De Leo, Sun Y Lee, Lewis E Braverman
The Lancet.2016; 388(10047): 906. CrossRef - Differentiating Graves' disease from subacute thyroiditis using ratio of serum free triiodothyronine to free thyroxine
Chutintorn Sriphrapradang, Adikan Bhasipol
Annals of Medicine and Surgery.2016; 10: 69. CrossRef - Management of hyperthyroid patients in dental emergencies: a case report
Kyung-Jin Lee, Wonse Park, Nan-Sim Pang, Jin-Hyung Cho, Kee-Deog Kim, Bock Young Jung, Eun-Jung Kwak
Journal of Dental Anesthesia and Pain Medicine.2016; 16(2): 147. CrossRef - The Presence of Thyroid-Stimulation Blocking Antibody Prevents High Bone Turnover in Untreated Premenopausal Patients with Graves’ Disease
Sun Wook Cho, Jae Hyun Bae, Gyeong Woon Noh, Ye An Kim, Min Kyong Moon, Kyoung Un Park, Junghan Song, Ka Hee Yi, Do Joon Park, June-Key Chung, Bo Youn Cho, Young Joo Park, Jung-Eun Kim
PLOS ONE.2015; 10(12): e0144599. CrossRef - Refractory Graves' Disease Successfully Cured by Adjunctive Cholestyramine and Subsequent Total Thyroidectomy
Yeoree Yang, Seawon Hwang, Minji Kim, Yejee Lim, Min-Hee Kim, Sohee Lee, Dong-Jun Lim, Moo-Il Kang, Bong-Yun Cha
Endocrinology and Metabolism.2015; 30(4): 620. CrossRef - Improved quality of life in hyperthyroidism patients after surgery
Branka Bukvic, Vladan Zivaljevic, Sandra Sipetic, Aleksandar Diklic, Katarina Tausanovic, Dragos Stojanovic, Dejan Stevanovic, Ivan Paunovic
Journal of Surgical Research.2015; 193(2): 724. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Effect of previous administration of potassium iodine and different durations of low iodine diets for radioiodine therapy on the treatment of Graves' disease in iodine-rich areas


 KES
KES

 First
First Prev
Prev



